
- HOME
- Affective Disorders Research Project
Affective Disorders Research Project
Development of novel biomarkers and therapies for affective disorders
Research Summary
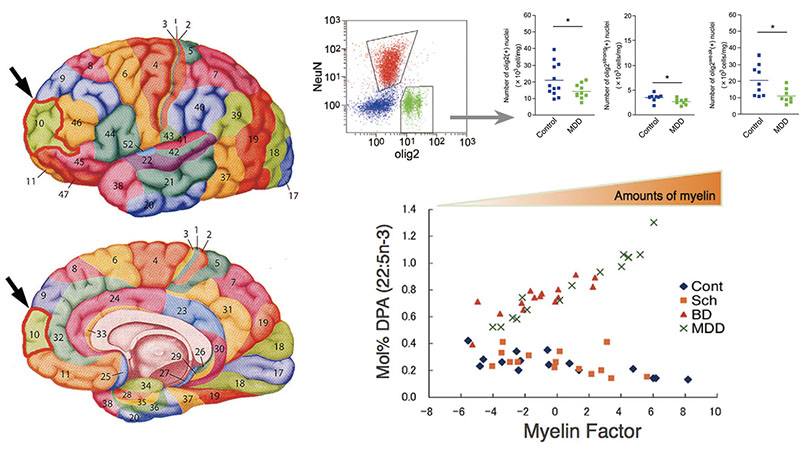
Major depressive disorder (MDD) and bipolar disorder (BD), collectively known as affective disorders, are relapsing and remitting disorders of affect with nearly full recovery between episodes. We use human postmortem brains and animal and cell culture models to identify the processes in which stress or aging causes changes in the brain to induce these disorders. An initial focus of our work was stress-induced or age-related changes in cellular structure and lipid composition, particularly in oligodendrocyte cells within the brain’s mood circuitry. We are also interested in the biological relationship between affective disorders and dementias such as Alzheimer’s disease.
We recently established a novel rat social defeat stress (SDS) model that develops prolonged MDD-like maladaptive social avoidance and sleep abnormalities. These abnormalities were associated with changes in electroencephalography (EEG) spectral powers, including reduced REM sleep theta power. Chronic treatment with two different classes of antidepressants (ADs), imipramine and fluoxetine, as well as preventative use of ergothioneine, a metabolite of the gut bacterium Lactobacillus reuteri, significantly ameliorated these behavioral, sleep, and EEG abnormalities.
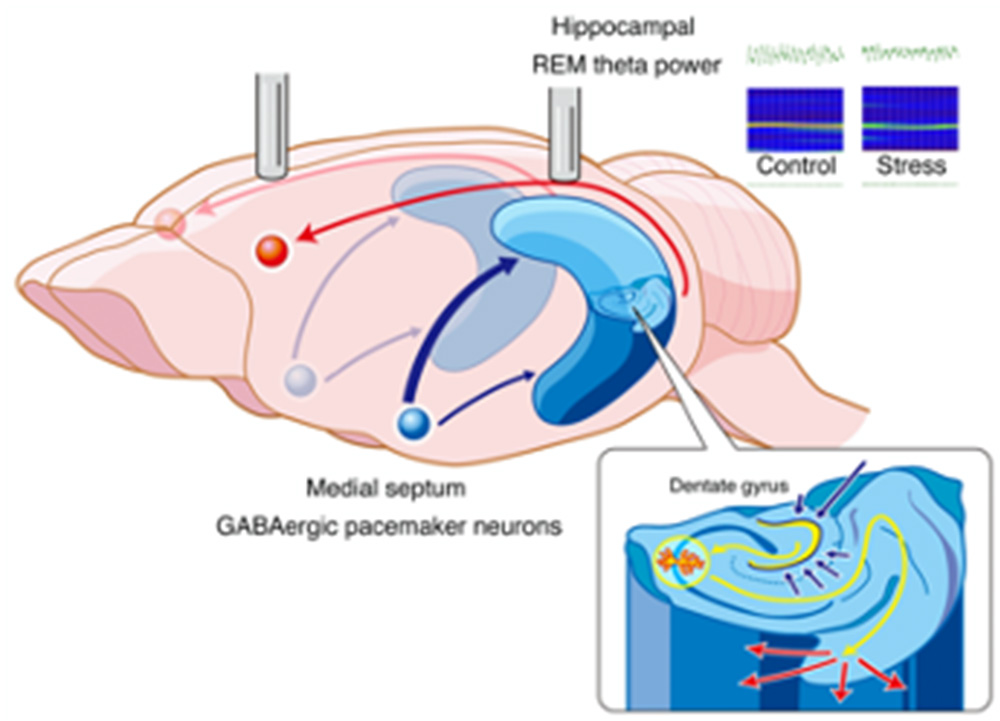
Interestingly, REM theta power was normalized by chronic but not acute AD administration. We speculate that the septohippocampal pathway, including the medial septum and hippocampus, may be partially or largely impaired by SDS, resulting in both emotional and/or cognitive symptoms in our model.
Inflammation may be involved in this process since ergothioneine has a strong anti-oxidative as well as anti-inflammatory effects.
Selected Publications
- Matsuda Y, et al. (2020) “Ergothioneine, a metabolite of the gut bacterium Lactobacillus reuteri, protects against stress-induced sleep disturbances.” Transl. Psychiatry 10:170.
- Bauer M, et al. (2014) “Relationship between sunlight and the age of onset of bipolar disorder: an international multisite study.” J. Affect. Disord. 167:104-111.
- Nihonmatsu-Kikuchi N, et al. (2013) “Depression and Alzheimer’s disease: novel postmortem brain studies reveal a possible common mechanism.” J. Affect. Disord>. 37: 11-21.
- Tatebayashi Y, et al. (2012) “Abnormal fatty acid composition in the frontopolar cortex of patients with affective disorders.” Transl. Psychiatry 2:e204.
- Hayashi Y, et al. (2012) “Neuropathological similarities and differences between schizophrenia and bipolar disorder: a flow cytometric postmortem brain study.” PLoS One 7: e33019.
- Hayashi Y, et al. (2011) “A novel, rapid, quantitative cell-counting method reveals oligodendroglial reduction in the frontopolar cortex in major depressive disorder.” Mol. Psychiatry 16: 1155-1158.

