
Toriumi K, Miyashita M, Yamasaki S, Suzuki K, Tabata K, Yamaguchi S, Usami S, Itokawa M, Nishida A, Kamiguchi H, Arai M. Itokawa M, Arai M. Association between plasma glucuronic acid levels and clinical features in schizophrenia. BJPsych Open. 2025. doi: 10.1192/bjo.2025.20.
doi: 10.1192/bjo.2025.20.
GlcA is an uronic acid formed by the oxidation of carbon at the C6 position of glucose. It is primarily synthesized in the liver via the uronic acid pathway and plays a crucial role in phase II metabolism through glucuronidation.
In our recent studies, we identified GlcA as a novel precursor of pentosidine (PEN) [1]. PEN is a type of advanced glycation end products (AGEs) known to accumulate in a subset of patients with schizophrenia (SCZ) [2]. Previous research has demonstrated an association between GlcA concentration and schizophrenia diagnosis, revealing that for one standard deviation (SD) increase in GlcA levels, the risk of developing schizophrenia nearly doubles. However, it remains unclear whether elevated GlcA levels directly contribute to the pathophysiology of schizophrenia, and the potential influence of medication has not been thoroughly examined.
In this study, we investigated the relationship between GlcA levels and clinical characteristics in patients with schizophrenia. Specifically, we assessed symptom severity using the PANSS and analyzed its correlation with GlcA concentrations. Additionally, to evaluate the impact of antipsychotic and psychotropic medication dosages on this association, we conducted multiple regression analyses.
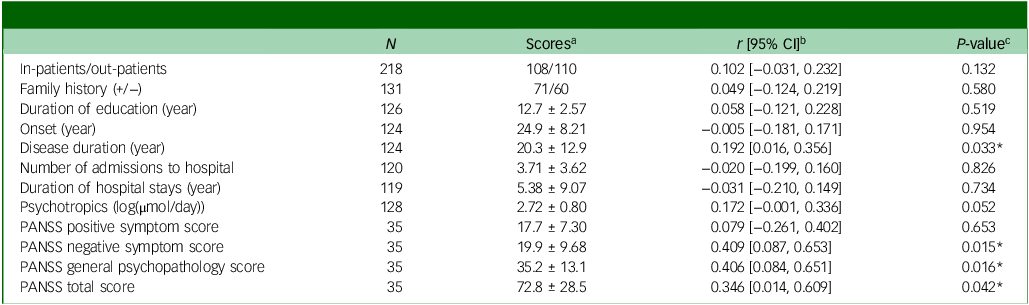
Given that GlcA is involved in the metabolism of a wide range of drugs, medication dosage could potentially influence GlcA levels. Additionally, previous studies have shown that GlcA levels increase with age [3]. To account for these factors, we conducted multiple regression analysis, which demonstrated that even after adjusting for age and psychotropic medication dosage (Table 2), GlcA levels remained significantly correlated with PANSS scores. These findings further support the potential involvement of GlcA accumulation in the pathophysiology of schizophrenia.
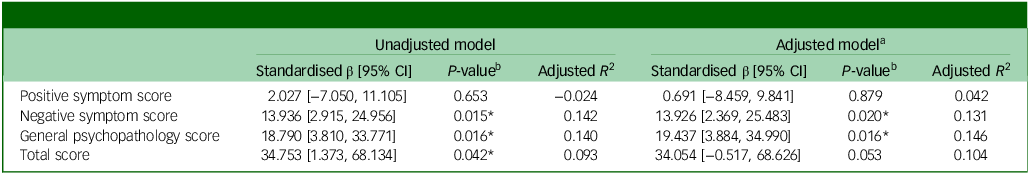
Overall, our study revealed a significant correlation between plasma GlcA levels and disease duration, as well as PANSS negative symptom scores, general psychopathology scores, and total scores in patients with schizophrenia. Furthermore, even after adjusting for age and psychotropic medication dosage, the significant associations between GlcA levels and PANSS negative symptom scores, as well as general psychopathology scores, persisted. Future research will aim to elucidate the molecular mechanisms by which GlcA influences schizophrenia symptoms. Additionally, we seek to explore targeted therapeutic interventions aimed at modulating GlcA levels to mitigate symptom severity and improve patient outcomes.