
Tabata K, Toriumi K, Suzuki K, Takagi H, Parida IS, Niizato K, Oshima K, Imai A, Nagase Y, Hashimoto R, Yamasaki S, Nishida A, Itokawa M, Takahashi H, Miyashita M, Arai M. Schizophrenia with hypozincemia: Clinical features and symptom severity Schizophr Res (2025) 286: 45915. doi: 10.1016/j.schres.2025.10.013
doi: 10.1016/j.schres.2025.10.013
SCZ is a heterogeneous psychiatric disorder with a complex and multifaceted pathophysiology, and no objective diagnostic biomarkers are currently available. A considerable proportion of patients present with negative symptoms or cognitive impairment that cannot be fully explained by the dopamine hypothesis, and approximately one-third show poor response to dopamine-targeting antipsychotic medications. These observations underscore the heterogeneity of SCZ and highlight the need to identify novel biomarkers that can delineate more homogeneous subtypes within the disorder.
Zn plays an essential role as a cofactor for numerous enzymes and transcription factors, and its deficiency can lead to a wide range of physiological dysfunctions, including immune abnormalities, delayed wound healing, and impairments in growth and neurodevelopment. Recent observational studies and meta-analyses consistently report reduced serum Zn levels in individuals with SCZ, particularly in first-episode and drug-naïve patients. Furthermore, analyses of hair and deciduous teeth suggest that Zn deficiency may already be present before the onset of illness.
However, it remains unclear how hypozincemia relates to the clinical features of SCZ or to the severity of psychiatric symptoms. If patients with low Zn levels represent a distinct and more homogeneous clinical subgroup—and if their symptoms can be ameliorated by Zn supplementation—this could provide important insights for more personalized approaches to diagnosis and treatment.
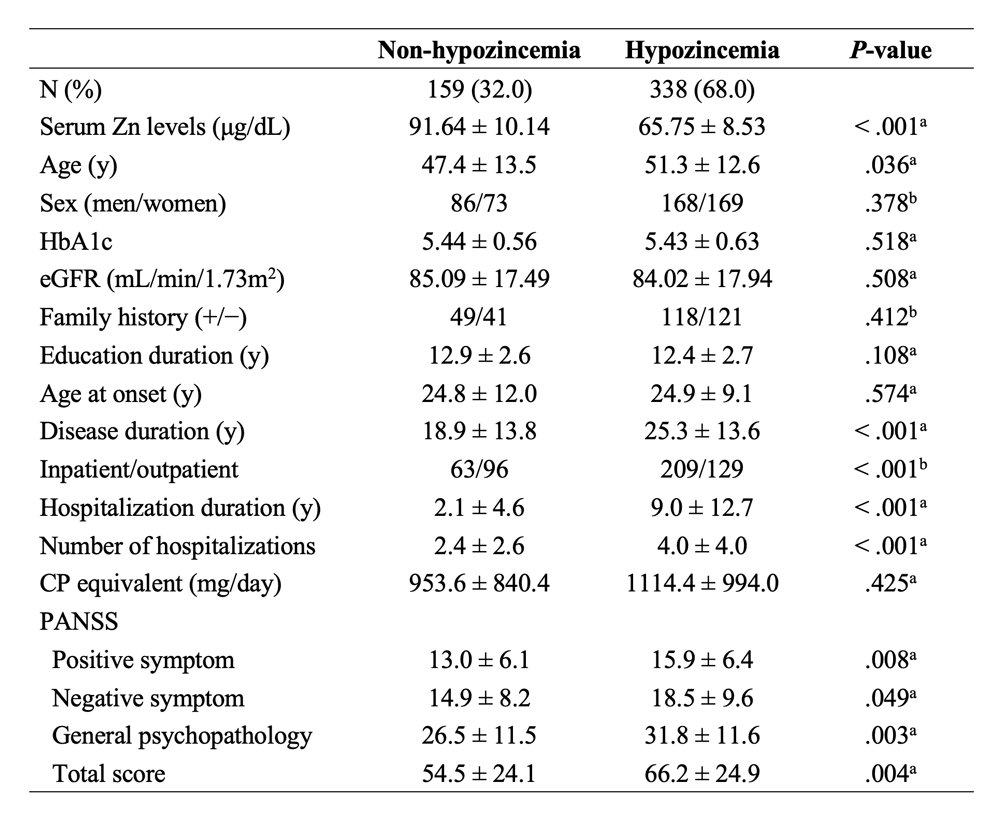
The aim of this study was to clarify the relationship between hypozincemia and clinical characteristics in patients with SCZ, and to test the hypothesis that serum Zn levels are associated with symptom severity as measured by PANSS scores.
Given that GlcA is involved in the metabolism of a wide range of drugs, medication dosage could potentially influence GlcA levels. Additionally, previous studies have shown that GlcA levels increase with age [3]. To account for these factors, we conducted multiple regression analysis, which demonstrated that even after adjusting for age and psychotropic medication dosage (Table 2), GlcA levels remained significantly correlated with PANSS scores. These findings further support the potential involvement of GlcA accumulation in the pathophysiology of schizophrenia.
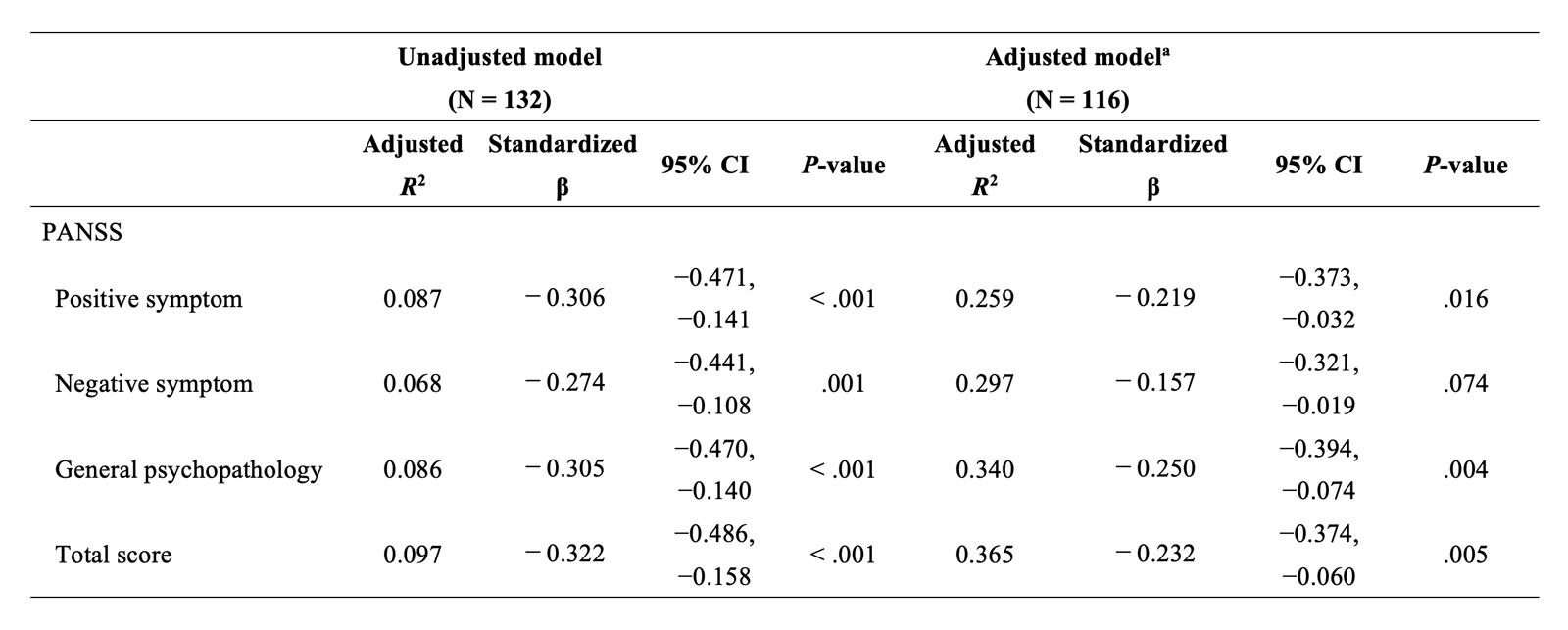
Overall, our study revealed a significant correlation between plasma GlcA levels and disease duration, as well as PANSS negative symptom scores, general psychopathology scores, and total scores in patients with schizophrenia. Furthermore, even after adjusting for age and psychotropic medication dosage, the significant associations between GlcA levels and PANSS negative symptom scores, as well as general psychopathology scores, persisted. Future research will aim to elucidate the molecular mechanisms by which GlcA influences schizophrenia symptoms. Additionally, we seek to explore targeted therapeutic interventions aimed at modulating GlcA levels to mitigate symptom severity and improve patient outcomes.