Meet our scientists!
 BackTopics Page
BackTopics Page
Psychiatric disorders are complex diseases that have a combination of genetic and environmental causes. While various genes that affect diseases such as schizophrenia and bipolar disorders have been identified, environmental contributions and the interactions between genetic and environmental effects that cause these diseases have not been as well-studied. Shinobu Hirai, a senior scientist in the department of Psychiatry and Behavioral Sciences has been studying how a combination of genetic and environmental influences can result in metabolic changes that cause psychiatric effects. Her latest results were published in a paper entitled, “High-sucrose diets contribute to brain angiopathy with impaired glucose uptake and psychosis-related higher brain dysfunction in mice” (Sci Adv. 7, eabl6077(2021)). We spoke to her about her work.

How did you first become interested in science?
My parents were both scientists. My father was a synthetic organic chemist, and my mother was a microbiological engineering chemist. When I was a child, they kept asking me questions about the world to stimulate my curiosity and increase my love for learning. In school, I loved my biology classes so I entered this field.
How did you become interested in diet and psychiatric diseases?
When I was in college, I lived on my own, and started eating a lot of sweets instead of eating a balanced diet. Because of this, I got sick, and my doctor told me to stop eating so poorly. After that I started eating more carefully and I became interested in how diets affect our mental health.
What was the start of your research for your Science Advances paper?
Patients with psychiatric diseases such as schizophrenia or bipolar disease eat much more sugar than healthy individuals, and those who eat more sugar tend to have more severe symptoms. Schizophrenia and bipolar disorders are caused by a complex interaction of genetic and environmental risk factors. From these observations, I decided to examine the connection between excess sugar consumption and psychosis-related behaviors.
Is there a connection between excess sugar consumption and psychiatric illnesses?
Yes! In my experiments, I used two different types of mice, one was a normal control and one expressed reduced amounts of GLO1, a protein that protects cells from oxidative damage. Reductions of GLO1 have been associated with schizophrenia. I fed these mice two types of diets. One was a high sucrose diet, and the other was a control starch-based diet. So, altogether I had a total of four different experimental conditions. When I looked at various behaviors, I found that GLO1 mutant mice fed high sucrose diets exhibited behaviors associated with schizophrenia and bipolar disorders, while mice in the three other conditions didn’t. Human schizophrenia and bipolar patients have changes in dopamine signaling in the brain and alterations in activity of certain neurons, called parvalbumin-positive neurons, and I found that GLO1 mutant mice fed high sucrose had similar changes. From these results, I concluded that a high sucrose diet can work in combination with a genetic predisposition to cause psychiatric disease.
How do high sucrose diets contribute to psychiatric diseases?
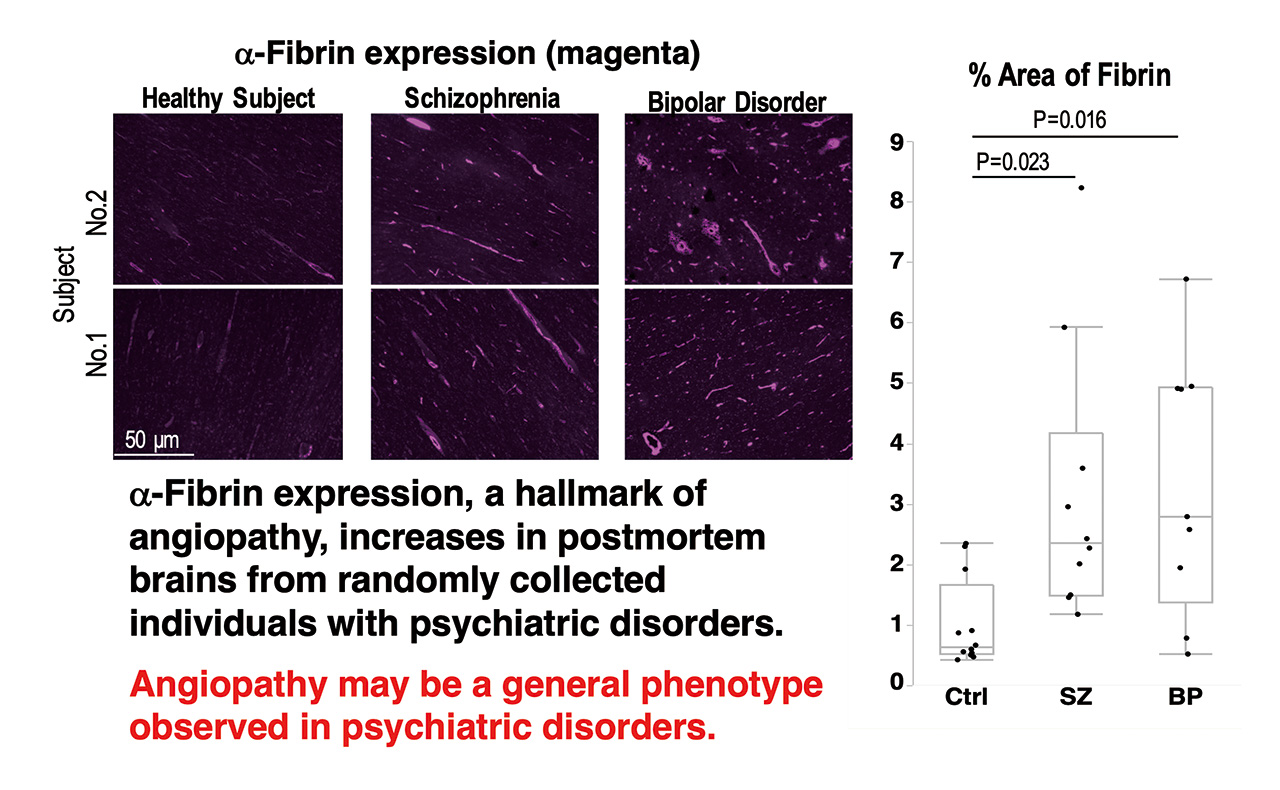
Both excess sucrose consumption and decreased GLO1 activity increase oxidative damage in our bodies. So, I thought that a combination of sucrose and decreased GLO1 could have additive or synergistic effects, and a large increase in oxidative stress could cause psychiatric illness. Indeed, I found a strong increase in oxidative damage, in blood vessels in brains of GLO1 mutant mice fed high sucrose. I also found that these mice had increased neuroinflammation and increased activation of immune cells and glia. These changes were accompanied by damage to the brain vasculature and decreased brain glucose. Interestingly, I found similar damage to the brain vasculature in the postmortem brains of schizophrenic and biopolar disorder patients. Overall, I think that oxidative damage to blood vessels decreases the amount of glucose transported to the brain. This leads to changes in brain activity and psychiatric illness.
How can we prevent damage to the brain vasculature?
Interestingly, I found that chronic low dose aspirin treatment prevents damage to the brain vasculature and rescues glucose uptake to the brain. It also decreased psychiatric behaviors. Aspirin suppresses inflammation and smoothens blood flow. I think it may also decrease accumulation of AGEs (Advanced Glycation End products).
What are your future plans?
Recently I’ve been studying how glucose is transported into the brain and I’ve obtained some fascinating results about a possible role for astrocytes. I’m really excited to pursue this research!