Abnormalities in glucose metabolism in the body cause non-enzymatic modifications called glycation (Maillard reactions) on proteins, nucleic acids, and lipids, forming advanced glycation end-products (AGEs). AGEs formation in biomolecules significantly affects their activity and physical properties. AGEs are also known to induce inflammatory responses via binding to a receptor for AGEs (RAGE). The adverse influence of AGEs accumulation is extensive throughout the body and can lead to various diseases. The inhibition of AGE formation is expected to be an effective preventive and therapeutic strategy for these diseases.
Pentosidine (PEN), a type of AGEs with fluorescence, possesses a cross-linked structure between lysine and arginine residues in proteins. PEN accumulation is associated with aging and various diseases such as diabetes mellitus, chronic kidney dysfunction, cataracts, osteoporosis, and Alzheimer’s disease. We previously reported that PEN levels in the peripheral blood of a subpopulation of patients with schizophrenia is significantly higher than that in healthy controls. Severe clinical features observed in patients with PEN accumulation, suggesting that PEN accumulation is one of the pathological mechanisms underlying schizophrenia.
It has been known that PEN is generated from glucose, fructose, pentose, and ascorbic acid. However, none of these substances was elevated in the subpopulation of patients with schizophrenia, although they had high PEN levels. In other words, it was unclear from what substance the increased PEN within patients was generated. Therefore, animal and cellular models that reproduce the pathophysiology of "PEN-accumulating schizophrenia" without increasing the already known PEN precursors have not been generated. Thus, the molecular mechanisms underlying the involvement of accumulated PEN in the pathophysiology of schizophrenia remain unclear.
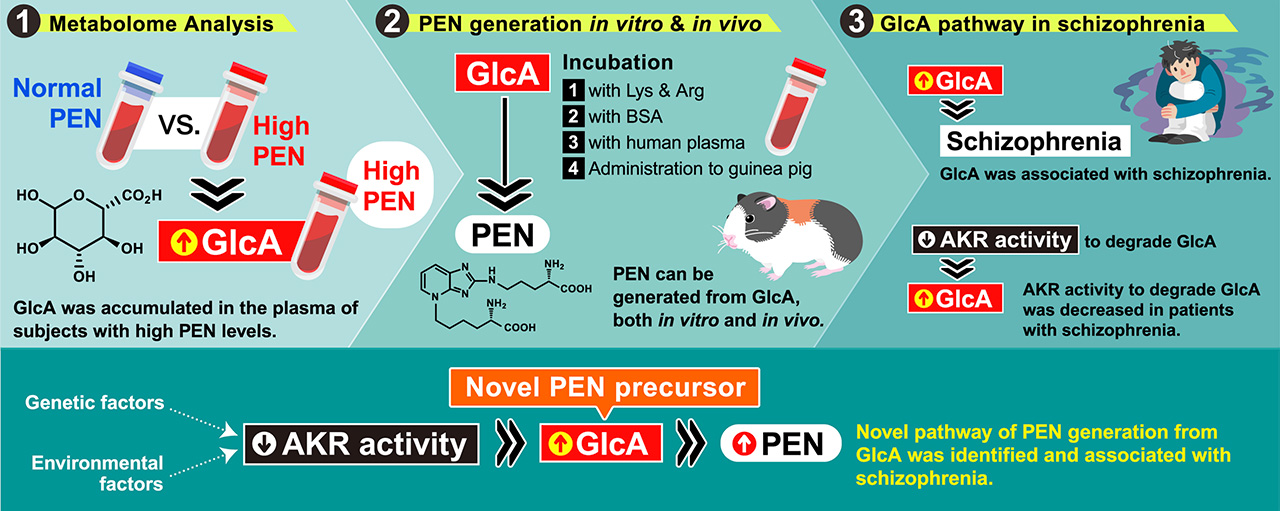
To identify novel precursors of PEN accumulated in patients with schizophrenia, we performed metabolome analysis using peripheral blood samples from two cohorts, including patients with high PEN levels. The results showed a significant accumulation of glucuronic acid (GlcA) in the high PEN group compared to the normal PEN group in both cohorts, and plasma PEN levels significantly correlated with plasma GlcA levels. Then, we found that PEN was generated by incubation of GlcA with lysine and arginine, BSA, or human plasma. We also demonstrated that GlcA treatment increased PEN levels in the plasma of guinea pigs but not in that of mice. Furthermore, GlcA has been associated with the diagnosis of schizophrenia. We showed that AKR activity to degrade GlcA was decreased in patients with schizophrenia, and its activity was negatively correlated with GlcA levels in the plasma, suggesting that the decreased AKR activity in patients with schizophrenia increases GlcA levels in the plasma, leading to PEN accumulation.
This is the first report to show that PEN is generated from GlcA. In the future, this finding will contribute to understanding the molecular pathogenesis of not only schizophrenia but also other diseases with PEN accumulation.